Have you ever felt heel pain? Not the kind of pain you get from blisters because the shoes you wore the other day were too tight, but the kind of persistent aching pain that can affect your mobility?
Heel pains aren’t necessarily a sign of any serious underlying condition, but it can interfere with some of your normal activities, especially exercise.

What causes heel pain?
Heel pain isn’t usually caused by an isolated instance of injury, such as twisting your ankle, falling, or stepping on a Lego brick. Rather, they usually result from repetitive stress and pressure on the heel.
They can also be caused by several conditions, such as plantar fasciitis, which is along the bottom of the heel, or Achilles tendonitis, which is along the back of the heel.
Possible causes of heel pain:
Plantar fasciitis
This condition is an inflammation of the plantar fascia, which is a tough ligament shaped like a bowstring that runs from your heel bone to the tip of your foot.
While the causes aren’t entirely clear, possible risk factors include standing for long hours and obesity, as well as excessive running and flat or high arches.
If you have plantar fasciitis, there is typically a sharp pain when you take your first few steps after getting out of bed, and it tends to improve with continued walking.
Heel bursitis
We have small sacs in our bodies called bursae, which help cushion our joints.
Bursitis occurs when these little sacs get inflamed and swollen, so heel bursitis refers to the condition when the bursa in the back of your heel gets inflamed.
It can result from landing awkwardly on your heel, or a particularly hard impact. Pressure from footwear can cause this too – such as poor-fitting shoes. You might feel this kind of pain deep inside your heel area, or at the back of it.
Tarsal tunnel syndrome
This occurs when a large nerve in the back of your foot becomes pinched or compressed. It’s a kind of compression neuropathy, and can be quite painful.
The nerve involved is known as the tibial nerve and is found along your inner leg behind the bump on the inside of your ankle.
You may have tarsal tunnel syndrome if you experience the following:
- Numbness in your foot that radiates outwards to your toes
- Tingling over the base of the foot
- Burning sensations and pain
Stress fractures
If you engage in a lot of activities that put a lot of stress on your feet, such as strenuous exercise, sports, or heavy manual work, you might experience this.
Those who do a lot of running are particularly prone to stress fractures in the bones of the foot. It can also be caused by osteoporosis.
Achilles tendonitis
This is when your Achilles tendon, which connects your calf muscles to your heel bone, gets injured from overuse.
It’s caused by repetitive or intense strain on the Achilles tendon, which is used for almost everything to do with movement – walking, running, jumping or standing on your toes.
This tendon also weakens as you get older, which makes it more vulnerable to injury. Sometimes, the tendon may not work properly because of multiple, tiny tears which can’t heal correctly.
Of course, there are other possible conditions that may cause you to feel pain in your heel too. In this table, we cover some of them and their potential causes.
| Condition | What is it? | Possible Causes |
| Bone tumors | Develop when cells within the bone divide uncontrollably, forming a lump or mass of abnormal tissue | – Genetics – Radiation treatment – Injury to bones |
| Haglund’s deformity | A bony enlargement on the back of the heel | – Possibly hereditary – High arches – Tight Achilles tendon – Tendency to walk on the outside of the heel |
| Heel spurs | Calcium deposits that cause bony protrusions on the underside of the heel bone | – Calcium deposit build-up on the underside of the heel bone |
| Achilles tendon rupture | Breakage of the Achilles tendon | – Sudden impact or trauma – Long term tendonitis |
| Osteomyelitis | A type of bone infection | – Bacterial infection |
| Paget’s disease of bone | Affects the way your body recycles bone tissue | – Slow viral infection – Hereditary factors |
| Peripheral neuropathy | Damage caused to nerves outside of the brain and spinal cord | – Range of causes depending on type of neuropathy |
| Reactive arthritis | Joint pain and swelling triggered by an infection in another part of your body | – Develops as a result of bacterial infection |
| Retrocalcaneal bursitis | Inflammation of bursae in the heel | – Friction against the heel bone from Achilles tendon rubbing over the bursa – Injury from falling or impact contusion |
| Rheumatoid arthritis | A type of inflammatory joint disease | – Autoimmune disease |
| Sarcoidosis | Collections of inflammatory cells in the body | Exact cause unknown, but theories include: – Genetics – Infectious agents – Autoimmune disorder |
How can I identify what’s causing the pain?
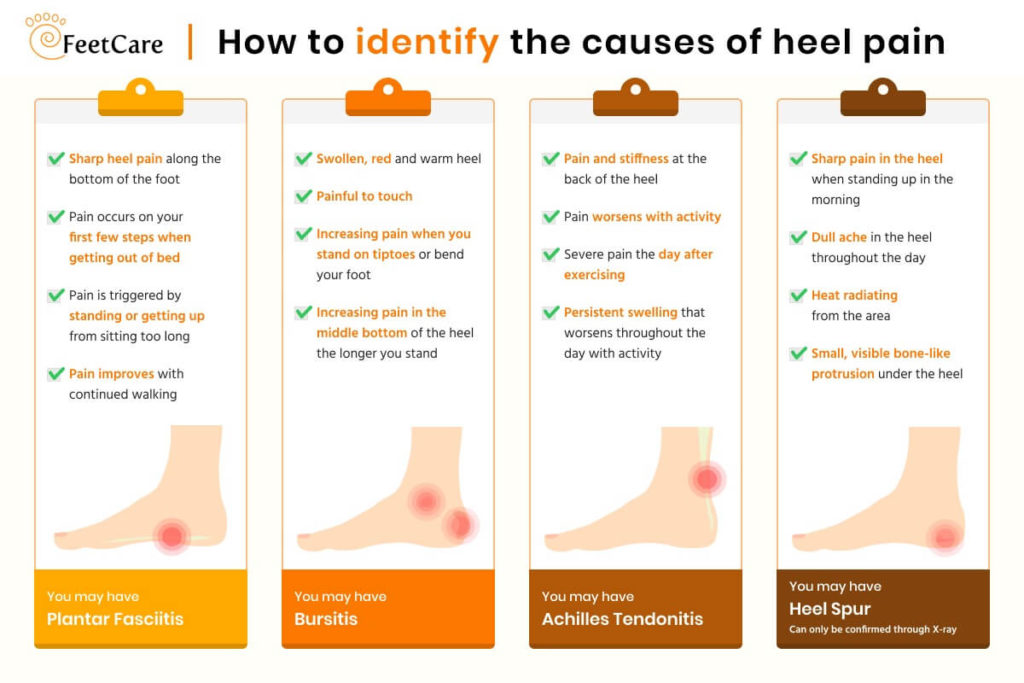
Plantar fasciitis
Intense heel pain along the bottom of the foot during the first few steps after getting out of bed in the morning. Often goes away once you start walking around, but may return in the late afternoon or evening.
Heel spur
May cause pain and tenderness on the undersurface of the heel that worsens over several months, but can only be confirmed through an X-ray.
Bursitis
Pain in the middle of the bottom of the heel that gets worse the longer you’re standing, and pain at the back of the heel that worsens if you bend your foot up or down.
Achilles tendonitis
Pain at the back of the heel where the Achilles tendon attaches. Typically becomes worse if you exercise or play sports, and usually followed by soreness, stiffness, and mild swelling.
Trapped nerve
Pain, numbness, or tingling almost anywhere at the back, inside, or bottom of the heel. In addition, you might see swelling or discoloration if the trapped nerve is due to a sprain, fracture, or other injuries.
How can I manage my heel pain?
In most cases, you can manage the pain with conservative treatments, though it will take a few months for recovery. Here are several options you can take.
1. Non-steroidal anti-inflammatory drugs (NSAIDs)
These are a type of painkillers that are derived from opioid-type drugs (such as morphine) and are used for less severe kinds of pain. They help reduce swelling and inflammation.
2. Corticosteroid injections
If NSAIDs prove to be ineffective, you can have the medication injected directly into the problem area.
You shouldn’t have them done more than a few times a year due to side effects such as:
- Acne, dry skin, or thinning skin
- Bruising or discoloration of skin
- Insomnia
- Mood changes
- Dizziness
- Increased sweating
- And many more
3. Physical therapy
Doing exercises that stretch the plantar fascia and Achilles tendon, and strengthen the lower leg muscles can result in more stable ankles and heels.
4. Orthotic devices and insoles
Getting fitted for orthotic devices and custom insoles can help correct foot problems. Proper cushioning and arch support also help speed up the healing process and might relieve some pain.
5. Getting adequate rest
Avoid activities that put lots of stress on your heels, like running and standing for long hours.
6. Icing your feet
Use ice packs or a bag of frozen peas and ice your heel for 15 to 20 minutes three times a day.
7. Get proper footwear
Make sure your shoes fit properly, and give plenty of support for your feet.
If you do a lot of sports, get the right kind of shoes, and replace them when they wear out. Browse a variety of footwear to help support your heel pain here.
You can also consider extracorporeal shock wave therapy if conservative methods don’t work out. This kind of therapy aims sound waves at the affected area to encourage and stimulate healing.

How can I prevent myself from getting heel pains?
Heel pain isn’t entirely preventable, depending on the condition that causes it. However, you can still undertake some steps to reduce the chances of getting it.
- Wear proper footwear that fits right and supports your feet
- Do warm-up stretches before starting your exercises
- Pace yourself appropriately during physical activities
- Maintain a healthy weight
- Take breaks when your muscles start aching
When should I see a doctor?
If you experience any of the following, you should see your doctor as soon as you can. They will take x-rays of your foot, and also be able to diagnose what exactly is causing your pain.
- You experience severe pain and swelling near your heel.
- You can’t bend your foot downward, or stand on your toes.
- You can’t walk normally.
- You have a fever in addition to your heel pain.
- You experience numbness or tingling in your heel.
- You experience severe heel pain immediately after hurting the area.
- You feel pain in your heel even when you’re not walking or standing.
- You still feel heel pain even after you’ve tried resting, icing your feet, and other home treatments and it persists for several weeks.
If you’re unsure why your heel hurts, our FeetCare specialists are trained to assess your condition. We’re here to help. Give us a call today.